Current Projects

This project focuses on designing and developing innovative technologies to enhance various aspects of Emergency Medical Services (EMS), including real-time data collection, information sharing, care coordination, and decision-making. A significant challenge in this setting is that emergency care professionals typically perform hands-on examinations and treatments while managing high physical and cognitive workloads, which limits their ability to interact with computing devices during patient care. The high-pressure, fast-paced, and complex nature of EMS work demands computing systems that are intuitive, easy to use, and seamlessly integrated into existing workflows. To address these design challenges, my research involves emergency care providers in the system design process to develop cutting-edge solutions, such as AI-powered clinical decision support systems and hands-free smart glass technologies.
Grants: NSF CRII (2020-2022, PI, $175,000), AHRQ R21 (2021-2023, PI, $300,000), NSF CAREER Award (2023-2028, PI, $500,000), NIH R15 (2024-2027, PI, $419,294).

Almost half of adults in the United States have limited health literacy, or limited capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. Compared with those with adequate health literacy, patients with limited health literacy experience disparities in health care access and use of health information technology. Prior research has found that current technologies for managing and reporting personal health data, such as patient portals, do not provide enough, or the right, support to aid patient understanding their personal healthcare data (e.g., lab test results, clinical notes). It is unknown, however, how can we better support lay individuals with limited health literacy to read and comprehend their personal health data. To bridge this knowledge gap, this research will involve patients with limited health literacy and most at risk for poor health outcomes to develop mechanisms and novel technologies to promote the universal use of health information technology, and to aid them in managing, engaging with, and acting on personal health data.
Grants: AHRQ R21/R33 (2024-2029, co-I/site PI, $1,014,336), National a2Pilot Award (2025-2026, HCI Consultant, $280,000)

With the advances in artifical intelligence (AI) technology in recent years, the AI technology has been increasingly used in a variety of healthcare domains, such as decision support, health education, and self-diagnoses. Despite its high potential, there are still many issues in the use and adoption of AI systems by clinicians and patients. For example, a key usability challenge of these systems is the lack of explanations of their reasoning to the user, making it difficult for users to understand systems’ hidden intelligence and determine when it is appropriate to trust the system-generated recommendation (e.g., medical advice). This challenge is exacerbated due to the scale and complexity of today’s machine learning and AI technologies. More transparent interface has been proven as a promising means of increasing user’s awareness of system actions and logics. In this research, the focus is to understand how to design trust-inspiring, transparent intelligent systems to support effective human-AI interaction and collaboration in healthcare settings.
Past Projects
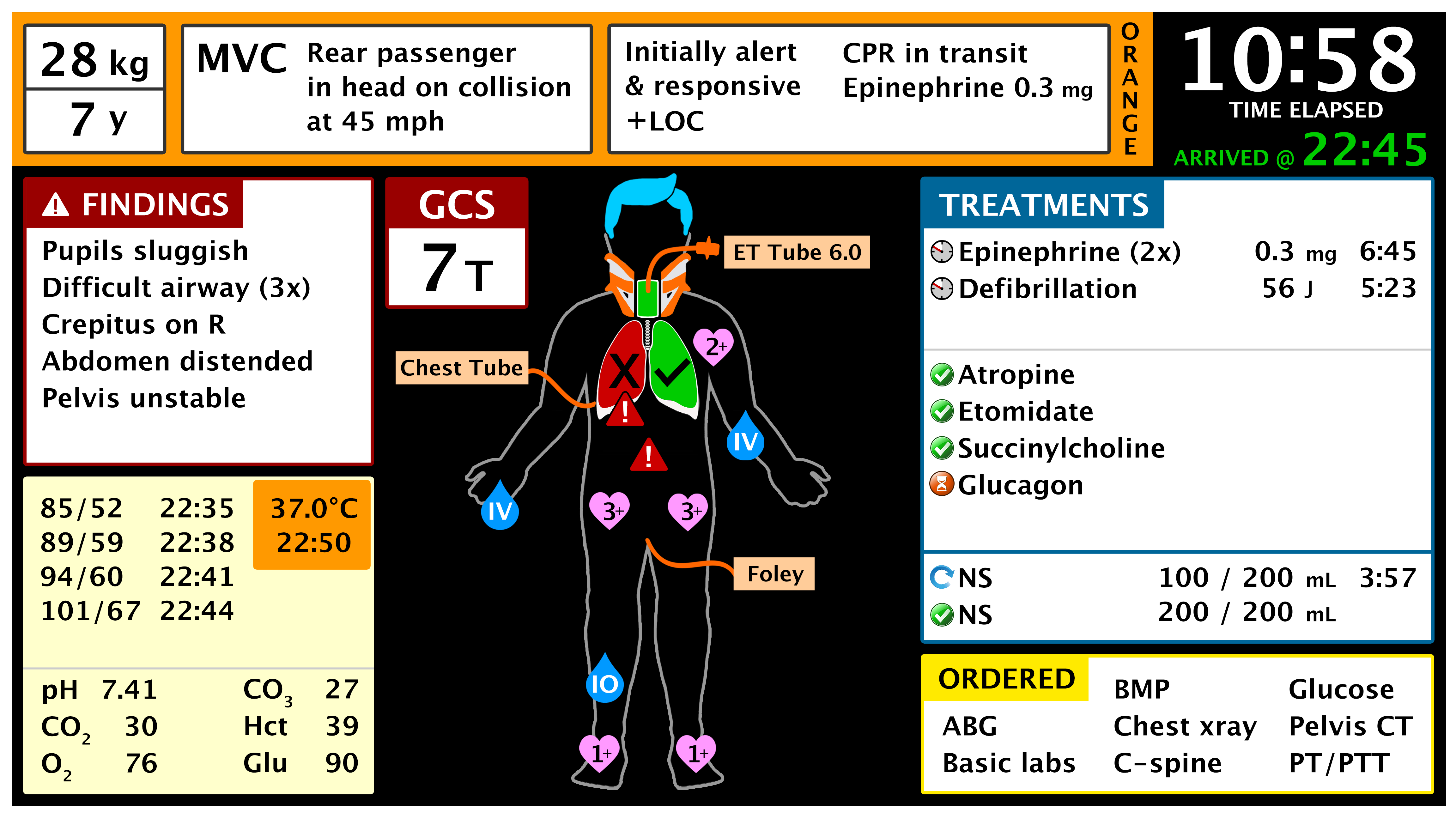
The goal of this project is to design and develop an integrated information capture and display system to support trauma team awareness and decision making.
We conducted comprehensive user studies (e.g., observations, focus groups and interviews) to identify problems of current work practice and understand trauma teams' information needs. Findings from those studies specify the rules for display design. Display is designed and developed using an iterative and user-centered design approach that combines participatory design workshops, rapid prototyping, and heuristic evaluation during simulated events.
Collaborators: Diana Kusunoki, Nadir Weibel, Ivan Marsic, Genevieve Tuveson, Randall Burd

Paper checklists have become increasingly common in healthcare and are now used to support a wide range of complex medical activities. This project aims to create dynamic digital checklist to support emergency medical work.
We analyzed a set of trauma resuscitation videos to evaluate and quantify effects of paper-based checklist on team communication and interaction behaviors. We also reviewed and analyzed hundreds of paper checklists collected from real resuscitations to identify use patterns of paper-based checklist. The research findings were translated into design implications for digital checklist.